COVID-19 mRNA vaccine makes tumors respond better to immunotherapy
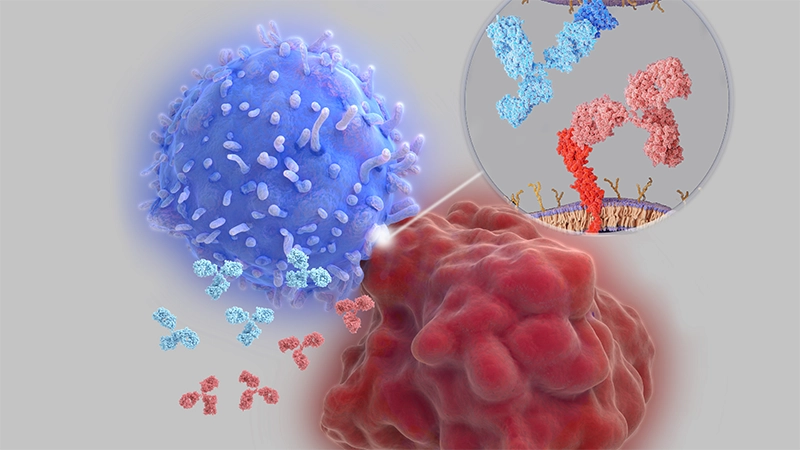
Recently, oncology researchers were energized by new findings published in Nature, showing that immune therapies such as nivolumab (Opdivo) and ipilimumab (Yervoy) may work better when given alongside an mRNA-based COVID-19 vaccine. These drugs are known as immune checkpoint inhibitors, which work by lifting the brakes on immune cells so they are free to attack the cancer cells.
The study published in Nature explores a fascinating interplay between routine mRNA vaccines originally developed for COVID‑19 and the effectiveness of immune checkpoint inhibitors (ICIs). Researchers found that administering an mRNA vaccine targeting the SARS-CoV-2 spike protein triggered a surge in type I interferon and activated innate immune cells, which in turn enhanced the priming of CD8+ T cells against tumor-associated antigens.
In animal models, combining this vaccination with ICIs led to significantly greater tumor regression than using either therapy alone—even in tumors classified as immunologically “cold,” meaning they typically don’t respond well to ICIs.
The human data in the paper offer a compelling translation of these findings. Patients with advanced non-small cell lung cancer (NSCLC) or melanoma who received a COVID-19 mRNA vaccine within 100 days of starting ICI treatment showed markedly improved overall survival compared with those who did not receive such a vaccine in that timeframe.
Moreover, tumor biopsies revealed that recent vaccination was associated with increased expression of PD-L1 in the tumor microenvironment, a change that may make the tumor more visible and vulnerable to ICI therapy.
This opens up a new concept: rather than vaccines only being used as prophylactic tools, they may act as immune system modulators to enhance cancer immunotherapy. Although the study was not conducted specifically for mesothelioma, this discovery is particularly exciting to mesothelioma researchers because the aforementioned immunotherapy treatment has shown better efficacy than previous treatment regimens but is still limited in its ability to extend survival.